- Subclassification of advanced-stage hepatocellular carcinoma with macrovascular invasion: combined transarterial chemoembolization and radiotherapy as an alternative first-line treatment
-
Sujin Jin, Won-Mook Choi, Ju Hyun Shim, Danbi Lee, Kang Mo Kim, Young-Suk Lim, Han Chu Lee, Jinhong Jung, Sang Min Yoon, Jonggi Choi
-
J Liver Cancer. 2023;23(1):177-188. Published online March 23, 2023
-
DOI: https://doi.org/10.17998/jlc.2023.03.04
-
-
1,495
Views
-
88
Downloads
-
3
Citations
-
 Abstract Abstract
 PDF PDF Supplementary Material Supplementary Material
- Background/Aim
The Barcelona Clinic Liver Cancer (BCLC) guidelines recommend systemic therapy as the only first-line treatment for patients with BCLC stage C hepatocellular carcinoma (HCC) despite its heterogeneity of disease extent. We aimed to identify patients who might benefit from combined transarterial chemoembolization (TACE) and radiation therapy (RT) by subclassifying BCLC stage C.
Methods
A total of 1,419 treatment-naïve BCLC stage C patients with macrovascular invasion (MVI) who were treated with combined TACE and RT (n=1,115) or systemic treatment (n=304) were analyzed. The primary outcome was overall survival (OS). Factors associated with OS were identified and assigned points by the Cox model. The patients were subclassified into three groups based on these points.
Results
The mean age was 55.4 years, and 87.8% were male. The median OS was 8.3 months. Multivariate analysis revealed a significant association of Child-Pugh B, infiltrative-type tumor or tumor size ≥10 cm, main or bilateral portal vein invasion, and extrahepatic metastasis with poor OS. The sub-classification was categorized into low (point ≤1), intermediate (point=2), and high (point ≥3) risks based on the sum of points (range, 0–4). The OS in the low, intermediate, and high-risk groups was 22.6, 8.2, and 3.8 months, respectively. In the low and intermediate-risk groups, patients treated with combined TACE and RT exhibited significantly longer OS (24.2 and 9.5 months, respectively) than those who received systemic treatment (6.4 and 5.1 months, respectively; P<0.0001).
Conclusions
Combined TACE and RT may be considered as a first-line treatment option for HCC patients with MVI when classified into low- and intermediate-risk groups.
-
Citations
Citations to this article as recorded by  - Liver resection in selective hepatocellular carcinoma with Vp3 or Vp4 portal vein tumor thrombosis improves prognosis
Manuel Lim, Jongman Kim, Jinsoo Rhu, Gyu-Seong Choi, Jae-Won Joh
Journal of Liver Cancer.2024; 24(1): 102. CrossRef - Comparison of atezolizumab plus bevacizumab and lenvatinib for hepatocellular carcinoma with portal vein tumor thrombosis
Jeayeon Park, Yun Bin Lee, Yunmi Ko, Youngsu Park, Hyunjae Shin, Moon Haeng Hur, Min Kyung Park, Dae-Won Lee, Eun Ju Cho, Kyung-Hun Lee, Jeong-Hoon Lee, Su Jong Yu, Tae-Yong Kim, Yoon Jun Kim, Tae-You Kim, Jung-Hwan Yoon
Journal of Liver Cancer.2024; 24(1): 81. CrossRef - How to optimize the treatment strategy for advanced-stage hepatocellular carcinoma with macrovascular invasion
Beom Kyung Kim
Journal of Liver Cancer.2023; 23(1): 121. CrossRef
- Stereotactic body radiation therapy for elderly patients with small hepatocellular carcinoma: a retrospective observational study
-
Jeong Yun Jang, Jinhong Jung, Danbi Lee, Ju Hyun Shim, Kang Mo Kim, Young-Suk Lim, Han Chu Lee, Jin-hong Park, Sang Min Yoon
-
J Liver Cancer. 2022;22(2):136-145. Published online September 16, 2022
-
DOI: https://doi.org/10.17998/jlc.2022.08.18
-
-
2,982
Views
-
73
Downloads
-
5
Citations
-
 Abstract Abstract
 PDF PDF Supplementary Material Supplementary Material
- Background/Aim
We aimed to investigate the efficacy and safety of stereotactic body radiation therapy (SBRT) in elderly patients with small hepatocellular carcinomas (HCC).
Methods
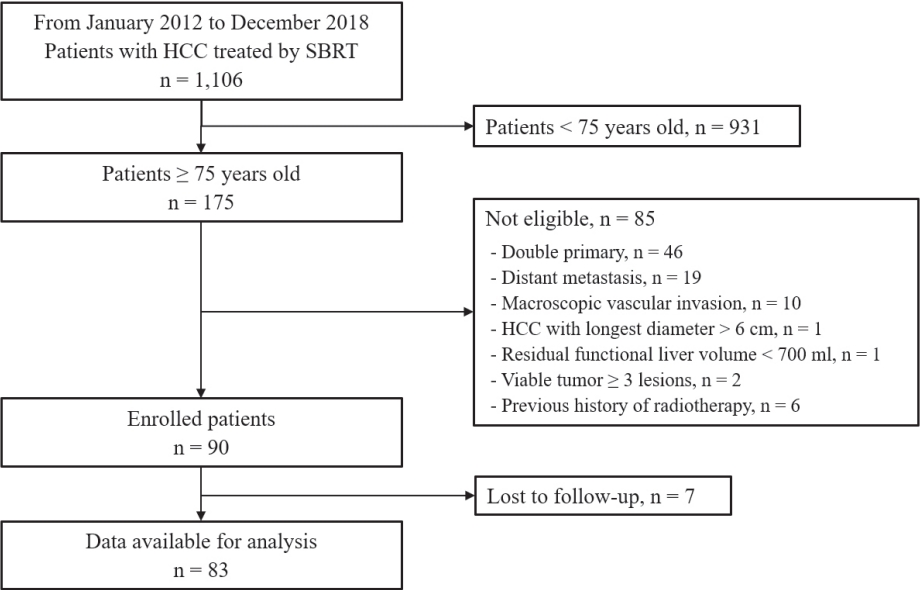
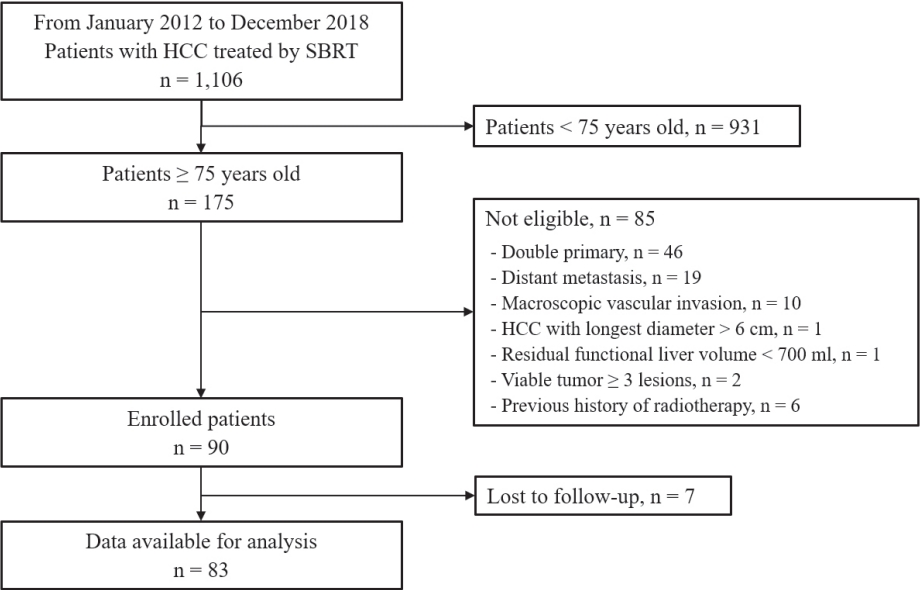
Eighty-three patients (89 lesions) with HCC who underwent SBRT between January 2012 and December 2018 were reviewed in this retrospective observational study. The key inclusion criteria were as follows: 1) age ≥75 years, 2) contraindications for hepatic resection or percutaneous ablative therapies, 3) no macroscopic vascular invasion, and 4) no extrahepatic metastasis.
Results
The patients were 75-90 years of age, and 49 (59.0%) of them were male. Most patients (94.0%) had an Eastern Cooperative Oncology Group performance status of 0 or 1. Seventy-four patients (89.2%) had Child-Pugh class A hepatic function before SBRT. The median tumor size was 1.6 cm (range, 0.7-3.5). The overall median follow-up period was 34.8 months (range, 7.3-99.3). The 5-year local tumor control rate was 90.1%. The 3-year and 5-year overall survival rate was 57.1% and 40.7%, respectively. Acute toxicity grade ≥3 was observed in three patients (3.6%) with elevated serum hepatic enzymes; however, no patient experienced a worsening of the Child-Pugh score to ≥2 after SBRT. None of the patients developed late toxicity (grade ≥3).
Conclusions
SBRT is a safe treatment option with a high local control rate in elderly patients with small HCC who are not eligible for other curative treatments.
-
Citations
Citations to this article as recorded by  - Radiofrequency Ablation versus Surgical Resection in Elderly Hepatocellular Carcinoma: A Systematic Review and Meta-Analysis
Jeong-Ju Yoo, Sujin Koo, Gi Hong Choi, Min Woo Lee, Seungeun Ryoo, Jungeun Park, Dong Ah Park
Current Oncology.2024; 31(1): 324. CrossRef - Radiotherapy trend in elderly hepatocellular carcinoma: retrospective analysis of patients diagnosed between 2005 and 2017
Bong Kyung Bae, Jeong Il Yu, Hee Chul Park, Myung Ji Goh, Yong-Han Paik
Radiation Oncology Journal.2023; 41(2): 98. CrossRef - Loco-regional therapies competing with radiofrequency ablation in potential indications for hepatocellular carcinoma: a network meta-analysis
Ha Il Kim, Jihyun An, Seungbong Han, Ju Hyun Shim
Clinical and Molecular Hepatology.2023; 29(4): 1013. CrossRef - Has the growing evidence of radiotherapy for hepatocellular carcinoma increased the use of radiotherapy in elderly patients?
Tae Hyun Kim
Radiation Oncology Journal.2023; 41(3): 141. CrossRef - Chronic Liver Disease in the Older Patient—Evaluation and Management
Daniel Anthony DiLeo, Tolga Gidener, Ayse Aytaman
Current Gastroenterology Reports.2023; 25(12): 390. CrossRef
- A Case of the Effective Treatment of HCC with Bile Duct Invasion and Portal Vein Thrombosis
-
Jihyun An, Danbi Lee, Ju Hyun Shim, Kang Mo Kim, Young-Suk Lim, Han Chu Lee, Young-Hwa Chung, Yung Sang Lee
-
Journal of the Korean Liver Cancer Study Group. 2013;13(2):169-172. Published online September 30, 2013
-
DOI: https://doi.org/10.17998/jlc.13.2.169
-
-
 Abstract Abstract
 PDF PDF
- Bile duct invasion of hepatocellular caricinoma (HCC) is rare, ranging from 1.2% to 9%. Moreover, the standard treatment of HCC with bile duct invasion is not yet established. We report a case of HCC with bile duct invasion and portal vein thrombosis which was successfully treated by trasarterial chemoembolization and radiotherapy. A 38-year-old female patient visited our hospital due to right upper quadrant pain. The level of total and direct bilirubin was 6.8 and 4.0 mg/dL, respectively. Her blood test showed HBs Ag positive and the level of alpha-fetoprotein was 43,000 ng/mL. Her CT scan revealed lobulating hypervascular mass involving right hepatic lobe, portal vein and both intrahepatic ducts. We performed endoscopic biliary drainage using biliary stent. She had been diagnosed as HCC on endobiliary biopsy. She was treated with radiotherapy (RT) to portal vein thrombosis, and seven transarterial chemoembolizations. After of all, we carried out radiotherapy to hepatic vein thrombosis and residual HCC near hepatic vein. After the RT, she has been taken care at outpatient clinic without evidence of recurrence during 8 months.
- A Case of Hemolytic Uremic Syndrome after Cisplatin Based Transarterial Chemoembolization
-
Chang Hyeon Seok, Danbi Lee, Ju Hyun Shim, Kang Mo Kim, Young-Suk Lim, Han Chu Lee, Young-Hwa Chung, Yung Sang Lee
-
Journal of the Korean Liver Cancer Study Group. 2012;12(2):169-171. Published online September 30, 2012
-
-
-
 Abstract Abstract
 PDF PDF
- Hemolytic uremic syndrome (HUS) is a rare condition compromising the clinical triad of acute renal failure, microangiopathic
hemolytic anemia, and thrombocytopenia. HUS may be associated with a variety of etiologies, and chemotherapeutic agents have
also been reported to be associated with HUS, including mitomycin, cisplatin, bleomycin, and most recently gemcitabine. HUS
also has been observed in association with a number of disseminated malignancies in adults, most typically adenocarcinoma of
the stomach and breast. But there was no case report of HUS after cisplatin based transarterial chemoembolization (TACE) for
hepatocellular carcinoma (HCC). We experienced a case of HUS after cisplatin based TACE and reported this case with several
literature reviews.
- A Case of Small HCC
-
Chang Hyeon Seock, Danbi Lee, Ju Hyun Shim, Kang Mo Kim, Young-Suk Lim, Han Chu Lee, Young-Hwa Chung, Yung Sang Lee
-
Journal of the Korean Liver Cancer Study Group. 2012;12(1):28-31. Published online February 28, 2012
-
-
-
 Abstract Abstract
 PDF PDF
- According to AASLD practice guideline, nodules that are smaller than 1 cm should be followed with ultrasound at intervals
from 3-6 months and nodules larger than 1 cm found on ultrasound screening of a cirrhotic liver should be investigated further
with either 4-phase multidetector CT scan or dynamic contrast enhanced MRI. If the appearances are typical of HCC, the lesion
should be treated as HCC. We experienced a patient who has a hepatic nodule smaller than 1 cm and followed AASLD guideline
and performed radiofrequency ablation for hepatocellularcarcinoma after 13 months later. MRI helped to diagnose hepatic
nodule as a hepatocellularcarcinoma during surveillance.
- A Case of a Advanced Stage Hepatocelluar Carcinoma Patient with Relatively Good Response after Combination Therapy
-
Chang Hyeon Seock, Danbi Lee, Ju Hyun Shim, Kang Mo Kim, Young-Suk Lim, Han Chu Lee, Young-Hwa Chung, Yung Sang Lee
-
Journal of the Korean Liver Cancer Study Group. 2012;12(1):58-61. Published online February 28, 2012
-
-
-
 Abstract Abstract
 PDF PDF
- According to AASLD practice guideline, for patients who present with advanced hepatocelluar carcinoma, new data indicates
the efficacy of sorafenib in prolonging life. But there are no data comparing combination transarterial chemoemboliation with
sorafenib to sorafenib treatment alone. We experienced a case that treated a patient with combination therapy including
transarterial chemoembolization for intrahepatic hepatocelluarcarcinoma, radiation therapy for portal vein thrombosis and
sorafenib treatment. He was in stable disease state after 6 months later. Therefore, it seems to be need to study for comparing
combination therapy to sorafenib, or to transarterial chemoembolization.
- A Case of Hepatocellular Carcinoma with Bile Duct Invasion
-
Danbi Lee, Kang Mo Kim, Young-Suk Lim, Han Chu Lee, Young-Hwa Chung, Yung Sang Lee, Dong Jin Suh
-
Journal of the Korean Liver Cancer Study Group. 2008;8(1):55-58. Published online June 30, 2008
-
-
-
 Abstract Abstract
 PDF PDF
- Bile duct invasion of hepatocellular carcinoma (HCC) is rare, ranging from 1.2% to 9 %. A 51-year-old male
patient visited our hospital due to jaundice. He had been infected with hepatitis B virus. He had icteric sclera
without abdominal distension or tenderness. The level of total and direct bilirubin was 16.7 and 7.8 mg/dL, each
other. The level of AFP was 4690 ng/mL. CT scan showed ill-defined hypervascular mass involving left hepatic
lobe, left intrahepatic duct and common hepatic duct. He had been diagnosed as HCC on liver biopsy. We
performed total 3 PTBDs in right, left lateral, and left medial side of the bile duct. After then, he was treated with
two transarterial chemoembolizations. Finally, we carried out extended left lobectomy. After the surgery, he has
been taken care at OPD without evidence of recurrence during 8 months.
- Outcomes of Liver Resection and Transarterial Chemoembolization in Patients with Multinodular BCLC-A Hepatocellular Carcinoma
-
Jiwon Yang, Won-Mook Choi, Danbi Lee, Ju Hyun Shim, Kang Mo Kim, Young-Suk Lim, Han Chu Lee, Deok-Bog Moon, Dong-Hwan Jung, Jonggi Choi
-
Received March 3, 2024 Accepted March 25, 2024 Published online April 3, 2024
-
DOI: https://doi.org/10.17998/jlc.2024.03.25
[Accepted]
-
-
 Abstract Abstract
 PDF PDF
- Background
This study aimed to compare the outcomes of liver resection (LR) and transarterial chemoembolization (TACE) in patients with multinodular hepatocellular carcinoma (HCC) within the Milan criteria who were not eligible for liver transplantation.
Methods
We retrospectively analyzed 483 patients with multinodular HCC within the Milan criteria, who underwent either LR or TACE as an initial therapy between 2013 and 2022. The overall survival (OS) in the entire population and recurrence-free survival (RFS) in patients who underwent LR and TACE and achieved a complete response were analyzed. Propensity score (PS) matching analysis was also used for a fair comparison of outcomes between the two groups.
Results
Among the 483 patients, 107 (22.2%) and 376 (77.8%) underwent LR and TACE, respectively. The median size of the largest tumor was 2.0 cm, and 72.3% of the patients had two HCC lesions. The median OS and RFS were significantly longer in the LR group than in the TACE group (p <0.01 for both). In the multivariate analysis, TACE (adjusted hazard ratio [aHR], 1.81 and aHR, 2.41) and large tumor size (aHR, 1.43 and aHR, 1.44) were significantly associated with worse OS and RFS, respectively. The PS-matched analysis also demonstrated that the LR group had significantly longer OS and RFS than the TACE group (PS <0.05).
Conclusion
In this study, LR showed better OS and RFS than TACE in patients with multinodular Barcelona Clinic Liver Cancer stage A HCC. Therefore, LR can be considered an effective treatment option for these patients.
|